In the realm of medical mysteries, a rare and baffling case has emerged that challenges our understanding of a notorious affliction – necrotizing fasciitis, colloquially known as the “flesh-eating” bacterial infection.
In a truly exceptional occurrence, a 58-year-old man battled this aggressive infection on both legs, but what sets this case apart is the staggering four-day gap between the infections taking root.
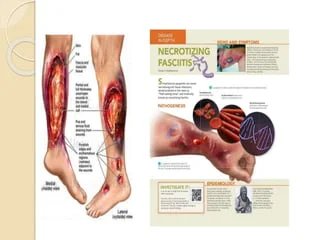
Necrotizing fasciitis is a nightmarish condition that propels bacteria to swiftly spread through the body, causing inflammation and tissue death. Historically, medical literature has indicated that the infection rapidly engulfs multiple sites within a short span of time.
However, the case reported from the University General Hospital Gregorio Marañon in Madrid has confounded medical experts by presenting a timeline that defies conventional wisdom.
The patient’s ordeal began with severe swelling, chest pain, and fever in his right leg. These ominous symptoms, hallmark indicators of necrotizing fasciitis, triggered a prompt response from medical professionals. A multidisciplinary approach will be adopted to encompass antibiotics, tissue removal, and the intricate fasciotomy procedure to alleviate swelling and pressure.
What makes this case truly unprecedented is the fact that, after battling and seemingly overcoming the infection in his right leg, the patient experienced a relapse – but on his left leg, and four days later.
Origination of the term
The term “metachronous necrotizing fasciitis” now finds its place in medical literature, describing the occurrence of this gruesome infection at separate times in different sites. The patient’s left leg displayed severe redness and blistering, indicative of the relentless bacterial assault.
Upon further examination, it was discovered that the same bacteria – Streptococcus pyogenes and Staphylococcus aureus – had managed to creep their way to the opposite leg.
Swift action is being taken, involving antibiotics including the removal of necrotic tissue, all in a bid to halt the infection’s advance. This peculiar case draws attention to the need for vigilance even after apparent recovery.
According to data from the Centers for Disease Control and Prevention (CDC), necrotizing fasciitis remains a formidable adversary, with an estimated 700 to 1,150 cases reported annually in the United States alone.
Disturbingly, even with treatment, the fatality rate looms at 20%, underscoring the urgency of early diagnosis and aggressive intervention.
Remarkably, against all odds, the medical team at University General Hospital Gregorio Marañon managed to triumph over this relentless infection.
Their diligence, combined with the patient’s resilience, led to a full recovery without the need for amputation or plastic surgery intervention.
This outcome underscores the importance of collaborative medical efforts and raises hope for those facing the daunting prospect of necrotizing fasciitis.
In conclusion, the curious case of metachronous necrotizing fasciitis challenges the boundaries of medical knowledge.
It serves as a reminder that even in the face of the most formidable adversaries, medical science’s dedication to understanding and conquering rare diseases continues to yield astonishing breakthroughs.